1. This Is Not the End
Sarah Zhang has an optimistic piece in the Atlantic, which argues that the end of the pandemic is now in sight.
This view is both right and wrong. Let’s start with the part that’s right. Here’s Zhang:
Pfizer and Moderna have separately released preliminary data that suggest their vaccines are both more than 90 percent effective, far more than many scientists expected. Neither company has publicly shared the full scope of their data, but independent clinical-trial monitoring boards have reviewed the results, and the FDA will soon scrutinize the vaccines for emergency use authorization. Unless the data take an unexpected turn, initial doses should be available in December.
The tasks that lie ahead—manufacturing vaccines at scale, distributing them via a cold or even ultracold chain, and persuading wary Americans to take them—are not trivial, but they are all within the realm of human knowledge. The most tenuous moment is over: The scientific uncertainty at the heart of COVID-19 vaccines is resolved. Vaccines work.
I would argue that Zhang overstates matters slightly in both directions.
The odds were always good that a vaccine would be workable and most of the early timelines suggested that the most likely scenario was a vaccine in wide distribution by summer of 2021. Which is about where we are heading.
I’m not sure that “persuading” Americans to take a COVID vaccine does fall within the realm of human knowledge. Public persuasion is more art than science and in this case it must work against an active resistance which is using new technologies to organize and spread misinformation.
And besides which: I am not prepared to accept as an absolute given that the Moderna and Pfizer vaccines are 100 percent going to wind up at the distribution stage. Are the chances that they clear the final hurdles in the neighborhood of 95 percent? Probably. But these chickens should not all be counted just yet.
With all of that said, Zhang’s overarching thesis is correct: The likely end of the pandemic is no longer hidden over the horizon. The zone of uncertainty regarding vaccine development has shrunk drastically. We can begin to plan for rebuilding with a good idea of where the hinge point will be rather than just making educated guesses, as we’ve been doing for the last 10 months.
So I want you to hold that idea in your head while you also consider the following:
We do not yet know how much pain and suffering we will experience between now and this “happy” ending.
Before we continue: We’re doing a livestream tonight to talk about what the Republican party should do—as well as what they will do, which are two different things—from here on out. It’s only for Bulwark+ members, so this would be a great time to join us.
2. The Paradox of Pain
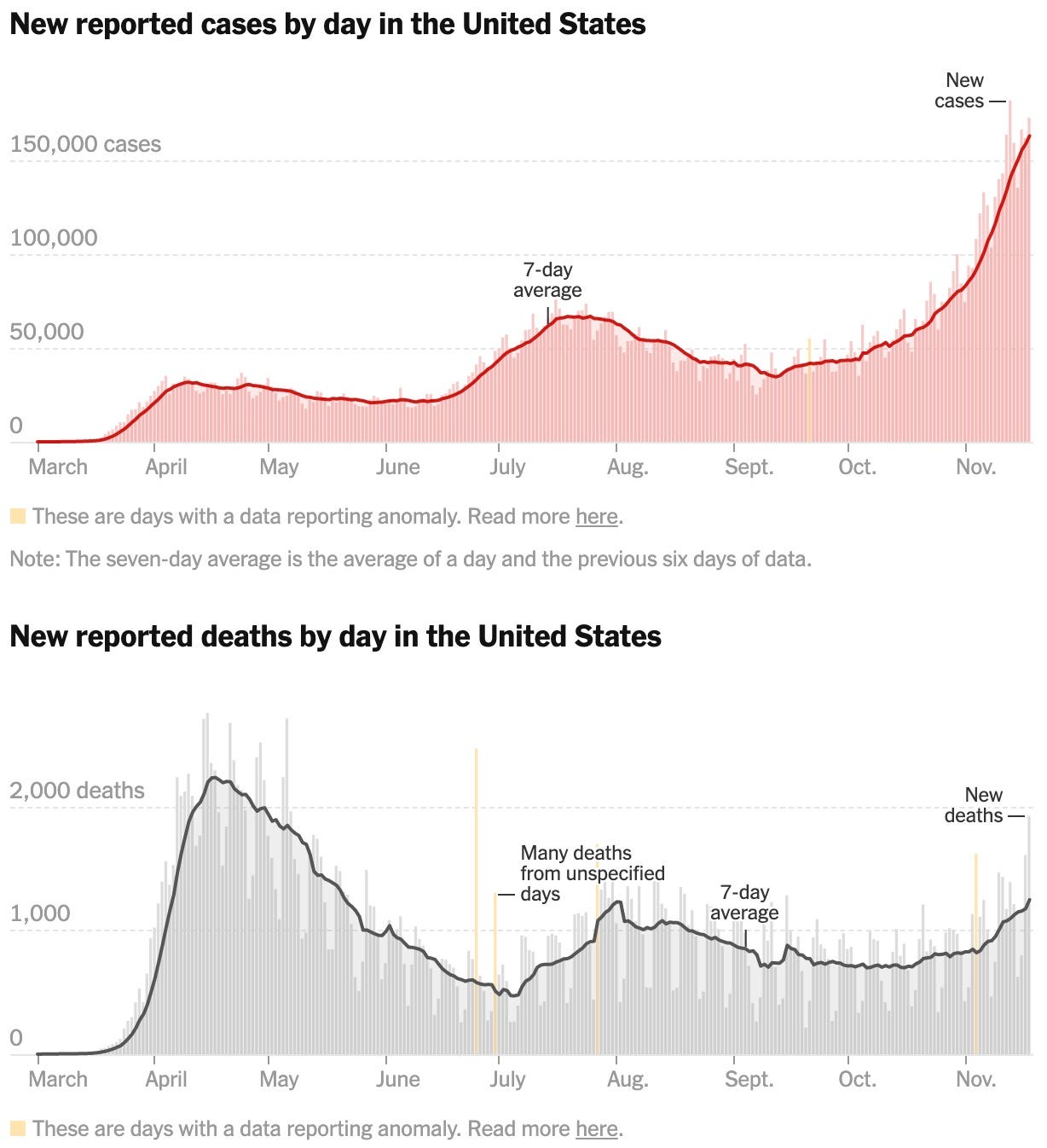
I want to share some graphics that, I hope, will scare the living shit out of you.
Look at the slope of the new-case curve. Now look at the slope of the new-deaths curve. And remember that the deaths always lag the case surge.
It is true that we’ve gotten better at treating COVID and lowered the case fatality rate. But the numbers are the numbers and you cannot “we-have-the-therapeutics” your way out of tens of thousands more dead Americans with numbers like we’re seeing. Yesterday alone we had 1,923 reported deaths.
Again: 1,923 dead people. In one day.
Where are things bad? Everywhere.
We are now well over a quarter million deaths in the United States. And wherever our final number will eventually settle, the total will be gruesome. We will almost certainly be over 300,000 by January. And then there will still be months to go before widespread availability of a vaccine.
Which is all the long way of saying that we are in this dangerous space where we face our moment of greatest peril at the same instant that we see the eventual end point.
But here’s the thing: We can choose to lessen the danger. It’s not that hard.
And yet, some people refuse to do it.
A week or two ago I got a note from a reader who is a healthcare professional who works in a hospital setting. She recounted to me how frustrated she has been because she finds herself treating seriously ill COVID patients who refuse to believe that they have COVID and who literally go to their deaths insisting that the pandemic is a Fake News Hoax perpetrated by Joe Biden, the Deep State, whomever.
I had hoped that her experiences were outliers. But I’m not so sure.
WTF is wrong with these people?
Remember John Kerry’s famous line about Vietnam: “How do you ask a man to be the last man to die for a mistake?”
That’s the point we’re at in the fight against COVID.
We never should have gotten here. America has only been ravaged at this magnitude because of the incompetence and malice of our president.
But the end is now in sight.
So when we talk about distancing, or mask mandates, or lockdowns, or mitigation strategies, we’re not projecting to infinity. We’re talking about a finite span of time with a firm-ish endpoint somewhere between 8 and 14 months from now.
Refusing to cooperate with public health measures now isn’t just unreasonable and dangerous. It’s an abomination. It’s asking someone to be the last person to die for Trump’s mistakes.
Stay home if you can. Wear a mask when you go out. Keep distance between yourself and others. Be mindful of ventilation.
We have it in our collective power to save lives between now and the time when vaccines are widely available.
But we can’t do it if a big chunk of the country is committed to unreality.
3. The N95 Supply Chain Failure
If ever there was a time for the federal government to step into a private sector market and take control of it, it was with the PPE shortages last spring. The NYT has a deep dive into what actually happened:
In his 30 years as a doctor, Andrew Artenstein had never worried about N95 respirators. The chief physician executive of Baystate Health, he ran his four hospitals in western Massachusetts exactingly, and an essential face covering being out of stock was inconceivable. His doctors, nurses and other responders went through about 4,000 a month, usually for treating patients with airborne diseases. There were always more in the warehouse, just outside the city of Springfield, where Baystate is based. But on April 6, as the novel coronavirus stampeded through the Northeast, Artenstein rose in predawn darkness, on a mission to secure about a quarter-million masks for his thousands of staff members. Baystate Health was just days away from running out.
For the next five hours, he was chauffeured down highways drained of normal traffic, while overhead a private plane bearing four specialists, who would vet the authenticity of the delivery, headed toward the same destination: a warehouse in the Mid-Atlantic, where the masks were being stored by a third-party dealer. A driver had been hired separately for Artenstein, because his frequent interactions with Covid patients meant he might expose the rest of the team to the virus. Two semitrailers were also converging to convey the delivery back to Massachusetts.
But it wasn’t actually clear yet how many N95 respirators there would be to pick up — the night before, the dealer confessed that he could only deliver a quarter of what had been promised, after canceling another pickup the previous week. (Because of an agreement between Baystate Health and the dealer, The Times has agreed not to identify him; he also declined to respond to questions.) Baystate Health had been forced to turn to unproven entrepreneurs like this after the corporate distributor it had once depended on ran out of N95s, when national and international supply chains collapsed at the beginning of the pandemic. Their predicament wasn’t unique. Many hospitals, states and even federal agencies were also desperate, transforming the normally staid market for health care commodities into a Darwinian competition of all against all.